|
It appears evident that the Endocannabinoid system is the Master control system for fine tuning all of our major body systems (immune, gastrointestinal, neurologic, metabolic) including the endocrine. There is evidence in the literature of dysfunction or involvement of the Endocannabinoid system in all endocrine functions and more broadly into metabolism. There is extensive literature and research into the ovarian, pancreas, adrenal, thyroid, hypothalamus – pituitary – adrenal system as well as the neural hormones. It appears that, in overview, the Endocannabinoid receptors are used to stimulate and inhibit endocrine function at a cellular level. In light of this all of endocrinology needs to be reorganized to incorporate a full understanding of the role of the Endocannabinoid system in modulating the endocrine subsystem.
1. CBD is a normalizing substance that restores homeostasis. The medical literature has identified over 30 mechanisms cannabidiol has used in modulating a particular physiologic function only a few of which were part of the Endocannabinoid system. CBD appears to correct for a a dysfunctional Endocannabinoid system and restore inter-and intracellular signaling. With those systems restored supplemental hormones could be more effective in individuals more responsive to smaller doses and less specific hormone combinations. 2. CBD does restore some function, inter and intracellular signaling and protects endocrine cells from further damage by oxidative substances as well as autoimmune disorders. There is suggestion in the literature for a regeneration of some endocrine cells, pancreatic beta cells for example but no evidence at this time. Let me give you an interesting example in that between 10 and 20% of men and women develop increased libido while taking cannabidiol. This even occurs with some geriatric patients over the age of 70. None of these behaviors appear to be extreme or outside of the physiologic range of normal. More accurately it could be described as a restoration of normal human behavior and function. At no time have I seen any abnormal or extreme behaviors or endocrine function. Philip Blair MD Medical Director for Elixinol, LLC
0 Comments
The harsh critique of the low-fat US dietary guidelines continues. Are they the result of an expert committee “completely dissociated from the top level scientific community”? That’s what one of the world’s top nutrition professors and researchers now says.
CardioBrief: Second Opinion on BMJ Dietary Guideline Takedown Here are the quotes from Professor Arne Astrup: …the committee seems to be completely dissociated from the top level scientific community, and unaware of the most updated evidence. There are now several new meta-analyses of both observational studies and also of randomized controlled trials clearly showing that there is no benefit of reducing saturated fat in the diet. All analyses and research can be criticized, but these meta-analyses have been published in leading scientific journals typically after critical reviews by three to five independent scientists (including a statistician), and by expert editors, so they cannot and should not be dismissed so easily.” Equally important, wrote Astrup, is “that the scientific studies that were the basis for the ‘cut down on saturated fat’ recommendations have been re-evaluated, and it is quite clear that today we would have concluded that there is no robust evidence to substantiate the advice.” “The same,” he continued, “applies to the importance of carbohydrate amount and source. Reducing total carbs or selecting the low glycemic index carbohydrates are well documented tools to produce weight loss and treat type 2 diabetes, and there is quite good evidence for efficacy and safety.” CommentIt’s quite clear there are big changes coming to the field of nutrition, and the old & moldy fear of fat is dying. Only question now is how long it’s going to take. Will the stalwart defenders of this failed idea make it to their retirement, or not, before it’s “game over” for them? Source: http://www.dietdoctor.com/is-the-us-dietary-guidelines-dissociated-from-scientific-community Date: May 26, 2016
Source: University of Southern California Summary: A mouse study, followed by a human study, indicates that the fasting-mimicking diet holds promise as a treatment for autoimmune diseases. A fasting-like diet switches on a process in which body kills bad cells, begins to generate new healthy ones, report scientists. Evidence is mounting that a diet mimicking the effects of fasting has health benefits beyond weight loss, with a new USC-led study indicating that it may reduce symptoms of multiple sclerosis. Scientists discovered that the diet triggers a death-and-life process for cells that appears critical for the body's repair. "During the fasting-mimicking diet, cortisone is produced and that initiates a killing of autoimmune cells," said Valter Longo, the study's lead author and professor who directs the USC Longevity Institute at the Davis School of Gerontology. "This process also leads to the production of new healthy cells." The new study, published in the journal Cell Reports, included mice and human patients who have multiple sclerosis. The neurological disease affects an estimated 350,000 Americans, according to the National Institute of Neurological Disorders and Stroke. Symptoms range from blurred vision to paralysis. These latest findings follow studies by the same USC lab that showed cycles of a similar but shorter fasting-mimicking diet, when paired with drug treatments for cancer, protect normal cells while weakening cancerous ones. In a separate study published last year, the lab found that the diet can cut visceral belly fat and reduce markers of aging and diseases in mice and humans. "We started thinking: If it kills a lot of immune cells and turns on the stem cells, is it possible that maybe it will kill the bad ones and then generate new good ones?" Longo said. "That's why we started this study." Study details For the first part of the study, researchers put a group of mice with autoimmune disease on a fasting-mimicking diet for three days, every seven days for three cycles, with a control group on a standard diet for comparison. Results showed that the fasting-mimicking diet reduced disease symptoms in all the mice, and "caused complete recovery for 20 percent of the animals," the researchers wrote. Testing the mice, the researchers found reductions in symptoms attributed to health improvements such as increased levels of the steroid hormone, corticosterone, which is released by the adrenal glands to control metabolism. They also saw a reduction in the inflammation-causing cytokines -- proteins which order other cells to repair sites of trauma, infection or other pain. They also saw improvements in the white blood "T cells," responsible for immunity. Finally, the researchers found that the fasting-mimicking diet promotes regeneration of the myelin -- the sheath of proteins and fats that insulate nerve fibers in the spine and brain that was damaged by the autoimmunity. Myelin is critical for the conduction of nerve impulses through the nervous system. In patients with multiple sclerosis, malfunctioning T cells attack the myelin and damage nerve fibers. Interfering with that degeneration while also promoting regeneration is critical for slowing the disease's development, which is what the periodic, regular fasts appear to trigger. "On the one hand, this fasting-mimicking diet kills bad immune cells," Longo said. "Then, after the mice return to the normal diet, the good immune cells but also the myelin-producing cells are generated, allowing a percentage of mice to reach a disease-free state." The researchers also checked the safety and potential efficacy of the diet on people who have multiple sclerosis through a pilot trial with 60 participants with the disease, lead by Markus Bock at Charité University Hospital in Berlin. Eighteen patients were placed on the fasting-mimicking diet for a seven day cycle and then placed on a Mediterranean diet for 6 months. Also for six months, 12 participants were on a controlled diet, and 18 others were on a ketogenic diet (a high-fat diet). Those who received a fasting mimicking diet cycle followed by the Mediterranean diet and those on a ketogenic diet reported improvements in their quality of life, improvements in health, including physical and mental health. The researchers noted that the study is limited because it did not test whether the Mediterranean diet alone would cause improvements, nor did it involve a functional MRI or immune function analysis. Longo said the findings beg further investigation. Researchers should determine whether a fasting-mimicking diet could help patients with other autoimmune diseases, and they should test the diet's efficacy in larger clinical trials. Similar fasting-mimicking diets have been tested and found safe in trials. Longo said he believes patients with autoimmune disorders who are out of viable options should consult their doctors about the possibility of trying the diet or enrolling in a clinical trial that tests the diet's effect on autoimmune disorders. Longo said he has heard positive feedback from patients with disorders who tried the diet. "We are optimistic," Longo said. "What we don't want is patients trying to do this at home without involvement of their specialist or without understanding that larger trials are necessary to confirm that the diet, as a treatment, is effective against multiple sclerosis or other autoimmunities." Source: https://www.sciencedaily.com/releases/2016/05/160526151941.htm Cannabidiol could be highly effective in depression by providing immediate and sustained anti-depressant effects. New evidence suggests that depression is an inflammatory condition of the brain and closely associated with chronic inflammatory conditions like diabetes and rheumatoid arthritis. CBD is a superb anti-inflammatory agent that readily crosses the blood brain barrier to quench those fires. In addition recent studies have revealed another pathway for CBD to relieve depression by modulating mood altering neurotransmitters of serotonin and glutamate.Current medical treatments for depression typically take considerable time to take effect and are frequently associated with numerous undesirable side effects like weight gain and the risk of suicide. Until the drugs reach therapeutic levels in the blood stream the patient continues to suffer, sometimes for weeks. CBD appears effective in both immediate and extended application.
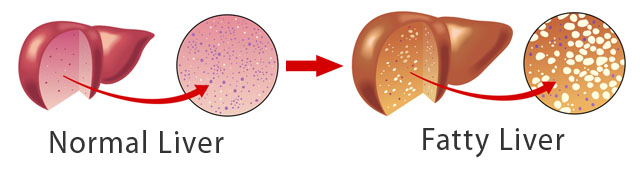
Depression is a state of low mood and aversion to activity that can affect a person's thoughts, behavior, feelings and sense of well-being. People with a depressed mood can feel many different ways. They may lose interest in activities that were once pleasurable, experience loss of appetite or overeating, have problems concentrating and may contemplate, attempt or commit suicide. Insomnia, excessive sleeping, fatigue, aches, pains, digestive problems or reduced energy may also be present. CBD appears to be effective for all of these symptoms. A medical literature review found 10 trials had evaluated the use of nonsteroidal anti-inflammatory drugs (NSAIDs) (n = 4258) and 4 investigated cytokine inhibitors (n = 2004). The pooled effect estimate suggested that anti-inflammatory treatment reduced depressive symptoms by 34% compared with placebo. JAMA Psychiatry. 2014;71(12):1381-1391. More science showed that the endocannabinoid (eCB) system, our personal endogenous lipid signaling system, appears to be disordered in depression. eCB is a potent modulator of immune system and could play a role in the chronic low-grade inflammation of depression. Psychopharmacology (Berl). 2015 Oct 20. In animal studies cannabidiol (CBD), exerts fast and sustained antidepressant-like effects through enhanced serotonin and glutamate levels. While chronic CBD exerted adaptive changes in pre- and post-synaptic 5-HT1A receptor functionality. Neuropharmacology. 2016 Apr;103:16-26. Dr. Blair comments: Clients with depression using CBD have frequently reported immediate and lasting benefit from the use of CBD without side effects allowing the immediate tapering of other medications without withdrawal symptoms or relapse. In addition to mood improvement other changes also occur in activity, sleep, energy, socialization and communication. Underlying inflammatory conditions, perhaps in lifestyle, should be addressed to sustain the benefits and reduce the need for CBD. Acute dose: 30mg/day, adjust to specific needs, taper other drugs after improvement. Study: Cannabidiol induces rapid-acting antidepressant-like effects and enhances cortical 5-HT/glutamate neurotransmission: role of 5-HT1A receptors. “My doctor says I have a fatty liver and I should stay away from fat,” writes this week’s house call. “Are high-fat foods the culprit here? Any tips to help with a fatty liver?”
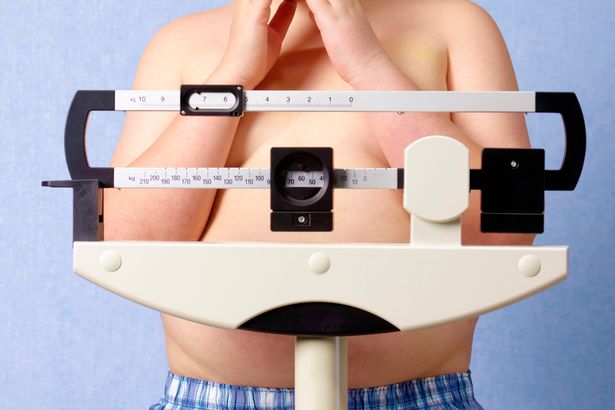
Indeed, your doctor is right to feel concern: Fatty liver is a dangerous yet misunderstood disease. In America, it affects 90 million of us and 17 percent of our children. Think about foie gras, the French delicacy made from duck or goose liver. It is made by force-feeding the animals a combination of sugar with corn and starch (a really sad, horrible practice), intentionally creating a fatty liver. So if you’re gorging on sugar and starch, you’re essentially doing the same thing with your own liver. Fatty liver literally means your liver fills with fat, paving the path for chronic disease and inflammation. You might be surprised to learn the primary culprit here. Research shows that carbs (and not fat) produce more fat in your belly and liver. Sugar switches on fat production in your liver, creating an internal process called lipogenesis, which is your body’s normal response to sugar. Fructose, the most detrimental sugar that heads directly to your liver, actually ramps up lipogenesis. That explains why sugar, especially fructose, becomes the chief cause of liver disease and the leading cause of liver transplants. What’s so bad about having a fatty liver? Well, among its numerous repercussions include inflammation, which triggers insulin resistance and pre-diabetes, meaning your body deposits fat in your liver and organs including your belly (called visceral fat). It gets worse. Excess sugar and starch creates more serious problems including high triglycerides, low HDL (“good” cholesterol), and high amounts of small LDL (dangerous cholesterol particles that cause heart attacks). Fatty liver also increases your heart attack risk. Sadly, most people have no idea they have a fatty liver. Today we’re even seeing 12-year-old boys with fatty livers because they guzzled soda for years and now need liver transplants. Fructose, the primary sweetener in sodas, is a key player in the ever-increasing rates of nonalcoholic fatty liver disease (NAFLD). We’re feeding children fructose and other highly toxic substances, setting the dismal stage for liver transplants, high blood pressure, diabetes, heart disease and abnormal cholesterol. Doctors then prescribe numerous medications to alleviate these and other issues. Overall, it becomes a bleak picture. I mentioned earlier sugar, not fat, creates fatty liver. Here’s where it gets interesting: Dietary fat actually turns off the fat production factory in your liver. You see, unlike carbohydrates and protein, dietary fat does not trigger your pancreas to secrete insulin or stress out your liver. Your body prefers to burn rather than store dietary fat, unless you combine it with carbs. When you eat the right fats, you increase your metabolism, stimulate fat burning and decrease hunger. One of my favorite fats is medium-chain triglycerides or MCTs, either in coconut oil or as a stand-alone oil. To prevent or reverse fatty liver, you’ll want to cut processed carbs and increase healthy fat intake, especially saturated - yes, saturated - fats from healthy foods like coconut and grass-fed beef. I realize all of this might sound confusing. After all, our government tells us to limit saturated fats to 7 to 10 percent of our calories even with the updated dietary guidelines (which science doesn’t support, by the way). We’ve demonized saturated fat for so long that we’ve missed the purple elephant in the room: SUGAR. Thankfully, newer guidelines tell us to limit sugar intake, however, they don’t go far enough. These guidelines should be fine-tuned to include whole grains, which also break down into sugar in your body. According to current guidelines, you’re still supposed to get one-quarter of your calories from sugar to be healthy. Crazy, right? I discuss how fat can benefit your liver and many other dietary fat issues in Eat Fat, Get Thin, but the take-home message here is that healthy saturated fats lower inflammation when you eat them as part of a low-carb, high-fiber, omega 3 fatty acid-rich diet. So how do you know if you have a fatty liver? If you eat lots of sugar and flour, have a little bit of belly fat, or if you crave carbs, you probably have a fatty liver. To heal that fatty liver and avoid its vast detrimental repercussions, you want to get to the root of those problems. Blood tests and an ultrasound can both detect fatty liver. If your blood test comes back abnormal, you must take it seriously. Even if your test comes back normal, don’t think you’re off the hook. A liver function test doesn’t always detect a fatty liver. An ultrasound is more sensitive. Fortunately, you can employ some simple but powerfully effective strategies to reverse or prevent fatty liver. I’ve found these diet, exercise and supplement strategies greatly benefit my patients. 1.Eliminate all high-fructose corn syrup (HFCS). Even when it comes in so-called healthy foods like salad dressings, don’t eat it. To put things into perspective, one serving of commercially made tomato sauce can have more fructose than a serving of Oreo sandwich cookies! 2.Get rid of white, processed flour and eliminate or greatly reduce starch. Even whole grain flours can be a problem. They increase your blood sugar levels, stressing your liver and resulting in high triglycerides, which promotes a fatty liver. 3.Add healthy fats. Functional Medicine becomes so simple: To heal the body, you remove the bad stuff and add in the good stuff. Incorporate anti-inflammatory, liver-healing foods like low-sugar fruit, vegetables, nuts, seeds, lean animal protein like chicken and fish and good, healthy fats like olive oil, macadamia nut oil, avocados, coconut oil, grass-fed butter and fish oil. A great way to combat sugar damage is to eat plenty of these healthy fats. You can get a powerful 21-day plan to easily incorporate healthy fats in Eat Fat, Get Thin. 4.Improve your metabolism through exercise. Routine, daily exercise improves insulin resistance and reduces fatty liver. Start out with something simple like walking 30 minutes. More seasoned exercisers might incorporate high-intensity interval training (or burst training) and weight lifting. 5.Supplement intelligently. The right supplements can help bring your body back into balance while it heals. Herbs like milk thistle are great for supporting the liver. I also use nutrients like lipoic acid and N-acetyl-cysteine, which make powerful antioxidants to heal and rejuvenate your liver while increasing the powerful antioxidant glutathione. Other liver-healing nutrients include B vitamins and magnesium. You can find these and other quality supplements in my store. 6.Eat detoxifying, liver-repairing super foods. Regularly eat foods from the cruciferous family - like broccoli, cauliflower and Brussels sprouts, as well as leafy veggies like kale, collards, cabbage, arugula, and watercress. At least a cup or two every day can help repair and heal the liver. Garlic and onions are amazing sulfur-rich foods that help detox the body. You’ll find amazing recipes and more ways to incorporate these amazing foods in The Blood Sugar Solution 10-Day Detox Diet. 7.Power up with protein. Protein at every meal, especially breakfast, becomes key to balancing blood sugar and insulin, cutting cravings and providing your liver the raw materials it needs to detoxify optimally. Start the day with farm fresh eggs or a protein shake. I recommend my Whole Food Protein Shake. Include nuts, seeds, eggs, fish, chicken or grass-fed meat for protein at every meal. A serving size is four to six ounces, or about the size of your palm. You need a healthy liver to combat toxic junk and chemicals in your environment. A healthy liver means your body stays healthy, you don’t get sick and you maintain plenty of energy. http://new.www.huffingtonpost.com/dr-mark-hyman/fatty-liver-is-more-dange_b_9952666.html DARWIN isn’t required reading for public health officials, but he should be. One reason that heart disease, diabetes and obesity have reached epidemic levels in the developed world is that our modern way of life is radically different from the hunter-gatherer environments in which our bodies evolved. But which modern changes are causing the most harm?
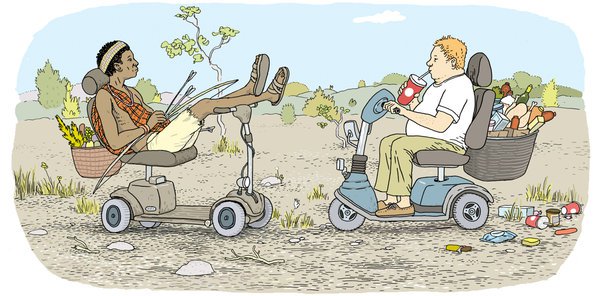
Many in public health believe that a major culprit is our sedentary lifestyle. Faced with relatively few physical demands today, our bodies burn fewer calories than they evolved to consume — and those unspent calories pile up over time as fat. The World Health Organization, in discussing the root causes of obesity, has cited a “decrease in physical activity due to the increasingly sedentary nature of many forms of work, changing modes of transportation and increasing urbanization.” This is a nice theory. But is it true? To find out, my colleagues and I recently measured daily energy expenditure among the Hadza people of Tanzania, one of the few remaining populations of traditional hunter-gatherers. Would the Hadza, whose basic way of life is so similar to that of our distant ancestors, expend more energy than we do? Our findings, published last month in the journal PLoS ONE, indicate that they don’t, suggesting that inactivity is not the source of modern obesity. Previous attempts to quantify daily energy expenditure among hunter-gatherers have relied entirely on estimation. By contrast, our study used a technique that calculates the body’s rate of carbon dioxide production — and hence the calories burned per day — by tracking the depletion of two isotopes (deuterium and oxygen-18) in an individual’s urine over a two-week period. It was a testament to the Hadza’s graciousness, and their years of friendship with several of my colleagues, that they welcomed us into their camps and participated in the study. As we sat back and observed, the Hadza went about their normal routines. The Hadza live in simple grass huts in the middle of a dry East African savanna. They have no guns, vehicles, crops or livestock. Each day the women comb miles of hilly terrain, foraging for tubers, berries and other wild plant foods, often while carrying infants, firewood and water. Men set out alone most days to collect honey or hunt for game using handmade bows and poison-tipped arrows, often covering 15 to 20 miles. We found that despite all this physical activity, the number of calories that the Hadza burned per day was indistinguishable from that of typical adults in Europe and the United States. We ran a number of statistical tests, accounting for body mass, lean body mass, age, sex and fat mass, and still found no difference in daily energy expenditure between the Hadza and their Western counterparts. How can the Hadza be more active than we are without burning more calories? It’s not that their bodies are more efficient, allowing them to do more with less: separate measurements showed that the Hadza burn just as many calories while walking or resting as Westerners do. We think that the Hadzas’ bodies have adjusted to the higher activity levels required for hunting and gathering by spending less energy elsewhere. Even for very active people, physical activity accounts for only a small portion of daily energy expenditure; most energy is spent behind the scenes on the myriad unseen tasks that keep our cells humming and our support systems working. If the Hadza’s bodies somehow manage to spend less energy in those areas, they could easily accommodate the elevated energy demands of hunting and gathering. And indeed, studies reporting differences in metabolic-hormone profiles between traditional and Western populations support this idea (though more work is needed). Our findings add to a growing body of evidence suggesting that energy expenditure is consistent across a broad range of lifestyles and cultures. Of course, if we push our bodies hard enough, we can increase our energy expenditure, at least in the short term. But our bodies are complex, dynamic machines, shaped over millions of years of evolution in environments where resources were usually limited; our bodies adapt to our daily routines and find ways to keep overall energy expenditure in check. All of this means that if we want to end obesity, we need to focus on our diet and reduce the number of calories we eat, particularly the sugars our primate brains have evolved to love. We’re getting fat because we eat too much, not because we’re sedentary. Physical activity is very important for maintaining physical and mental health, but we aren’t going to Jazzercise our way out of the obesity epidemic. We have a lot more to learn from groups like the Hadza, among whom obesity and heart disease are unheard of and 80-year-old grandmothers are strong and vital. Finding new approaches to public health problems will require further research into other cultures and our evolutionary past. Source: http://mobile.nytimes.com/2012/08/26/opinion/sunday/debunking-the-hunter-gatherer-workout.html?_r=0&referer When I was growing up in the 80s, New Kids on the Block were a massive hit. Yet, I never understood why, nor was I interested in their music. With behemoths like Michael Jackson and Milli Vanilli, who had time for NKOTB? In fact, I even saw Milli Vanilli live in concert and it was definitely one of my fondest childhood memories.
Granted, they were lip-syncing everything, but when you are 10 years old and a concert starts out with Rob and Fab battling in a sword fight, it is hard to get more exciting than that... With all the recent focus on carbohydrates in the diet and blood sugar, insulin, and the insulin receptor (the Fab Morvan, Rob Pilatus, and Michael Jackson of the metabolic world) the new kid on the block seems to be AMPK. AMPK, or AMP-activated protein kinase, is an enzyme extensively expressed in our skeletal muscle, liver, and brain. It serves as an energy regulator and this function is in response to several dietary and lifestyle habits. Amping up AMPK AMPK is basically an energy sensor that gets enhanced when our ATP is reduced (think of ATP as a transporter of energy) and AMP increases. ATP has three phosphates (the T is for tri) and when it loses one becomes ADP (the D is for di, or two) and when it loses two phosphates it becomes AMP (the M is mono for one). Without going too chemistry class on the reader, it can be simply viewed as: ATP → ADP + P ATP → AMP + 2P AMPK works to bring that AMP back up to ATP. In other words, AMPK acts to increase our available energy molecules. AMPK achieves this through several mechanisms described in the pictorial below. The dark blue mechanisms involve breaking down glucose (sugar) to burn for energy. This can be done by pulling glucose out of our bloodstream and placing it into our cells to be consumed. The aqua circles represent the breaking down of cholesterol and fat to be used as an efficient source of energy. The purple includes building more mitochondria to use these fats and sugars to make more energy, and the light blue mechanisms turn off cell building and replication. Basically, AMPK signals to our bodies and cells that it is not a time for building, but rather for breaking down and burning. AMPK and Cancer: AMPK is in essence the antithesis of cancer. While cancer cells are burning large amounts of glucose and nutrients, this is mostly to build up biomass — or, simply put, to keep growing and spreading. AMPK, on the other hand, shuts off this process, blocking cancer growth so we can feed our own cells.1,2 As you can see in the picture below, AMPK actually blocks mTOR, a pathway that leads to cancer survival and growth.3 This is the same pathway that is blocked with targeted cancer drugs. You will also notice in this picture that the pathways are all affected by intermittent fasting, labeled as “IF.” You may also notice that increased insulin sensitivity, which happens though exercise and a healthy diet, also appears to upregulate AMPK. AMPK and Warburg The Warburg hypothesis is something that comes up often around these parts. Very briefly put, Warburg showed that whether oxygen was present or not, cancer cells would rather use glucose for energy derivation. Even though when oxygen is present, cells can rely on mitochondria to make significantly more energy, cancer cells still seem to rely on the inefficient process of glycolysis (the breakdown of sugar).Well, while AMPK may stop cancer by blocking pathways like mTOR, newer data shows that it actually blocks the Warburg Effect by blocking the ability of cancer cells to use sugar for energy.4 Amping up AMPK The great thing about AMPK, is the plethora of ways we seem to be able to manipulate it. AmpK seems to take away the helplessness of disease or “luck” of cancer and lets us know that we do have biologic pathways that can clearly be manipulated by our lifestyle to thwart off disease. AMPK is upregulated via several mechanisms (in no apparent order):
Summing it up With all the recent talk of fasting, a ketogenic diet, and even calorie restriction, insulin (the hormone raised after carbohydrates are consumed in the diet) and the insulin-like growth factor receptor (where insulin and IGF bind) have been getting most of the hype. While it is well-deserved, as they are heavily implicated in cancer diagnosis and progression, we seem to be forgetting about AMPK, the new kid on the block. If we can increase an enzyme that helps stop cancer by fasting, limited carbs, and lifting some weights, isn’t the effect of lifestyle on health common sense at this point? And remember, even biochemically and metabolically, our lifestyles and actions translate to our health. While Milli Vanilli may not, AMPK helps prove this. References: 1. Shackelford DB, Shaw RJ. The LKB1-AMPK pathway: metabolism and growth control in tumour suppression. Nat Rev Cancer. 2009;9(8):563-575. doi:nrc2676 [pii] 10.1038/nrc2676. 2. Green AS, Chapuis N, Maciel TT, et al. The LKB1/AMPK signaling pathway has tumor suppressor activity in acute myeloid leukemia through the repression of mTOR-dependent oncogenic mRNA translation. Blood. 2010;116(20):4262-4273. doi:blood-2010-02-269837 [pii] 10.1182/blood-2010-02-269837. 3. Champ CE, Baserga R, Mishra M V, et al. Nutrient Restriction and Radiation Therapy for Cancer Treatment: When Less Is More. Oncologist. 2013;18(1):97-103. doi:10.1634/theoncologist.2012-0164. 4. Faubert B, Boily G, Izreig S, et al. AMPK is a negative regulator of the Warburg effect and suppresses tumor growth in vivo. Cell Metab. 2013;17(1):113-124. doi:10.1016/j.cmet.2012.12.001. 5. Vavvas D, Apazidis A, Saha AK, et al. Contraction-induced changes in acetyl-CoA carboxylase and 5’-AMP-activated kinase in skeletal muscle. J Biol Chem. 1997;272(20):13255-13261. http://www.ncbi.nlm.nih.gov/pubmed/9148944. Accessed January 16, 2015. 6. Winder WW, Hardie DG. Inactivation of acetyl-CoA carboxylase and activation of AMP-activated protein kinase in muscle during exercise. Am J Physiol. 1996;270(2 Pt 1):E299-E304. http://www.ncbi.nlm.nih.gov/pubmed/8779952. Accessed January 16, 2015. 7. Rasmussen BB, Winder WW. Effect of exercise intensity on skeletal muscle malonyl-CoA and acetyl-CoA carboxylase. J Appl Physiol. 1997;83(4):1104-1109. http://www.ncbi.nlm.nih.gov/pubmed/9338417. Accessed January 16, 2015. 8. Draznin B, Wang C, Adochio R, Leitner JW, Cornier MA. Effect of Dietary Macronutrient Composition on AMPK and SIRT1 Expression and Activity in Human Skeletal Muscle. Horm Metab Res. 2012;44(09):650-655. doi:10.1055/s-0032-1312656. 9. Cantó C, Jiang LQ, Deshmukh AS, et al. Interdependence of AMPK and SIRT1 for metabolic adaptation to fasting and exercise in skeletal muscle. Cell Metab. 2010;11(3):213-219. doi:10.1016/j.cmet.2010.02.006. Source: http://www.myhealthwire.com/news/herbs-supplements/963 During the years I practised as a hospital doctor I saw only one amputee. He’d had his lower leg amputated for bad circulation worsened by smoking . He wouldn’t give up his Woodbines, though, not even if his other leg was in jeopardy.
It’s a totally different picture today. Amputation is becoming commonplace – as a complication of diabetes. And no one seems worried. That’s because so many people are obese and it’s accepted as normal. Fat people develop Type 2 diabetes, and that, in turn, has become ‘normal’. People with Type 2 diabetes develop gangrene which often requires amputation and even that’s ‘normal’. Except it isn’t. Diabetes is perpetually in the news. It costs £10billion a year, a tenth of the total NHS budget. Britain now has an estimated four million diabetics, and many are undiagnosed. I find the lack of discussion about the consequences of diabetes terrifying. It has no cure and if it’s ignored, it will get worse. In Britain, diabetes causes 7,000 amputations a year – 135 legs are cut off every week and rising. Diabetes is nothing if not aggressive. It hurts every organ in the body. High blood sugar levels damage the delicate lining of small arteries leading to restriction of circulation to the legs. You lose sensation in your feet so if you stand on a pin, you won’t feel it. Infections are more virulent and poor circulation means antibiotics can’t reach the infection and amputation follows. According to Diabetes UK, 80% of amputations could be prevented. Dr Natasha Patel is a consultant in diabetes at Guy’s and St Thomas’ hospitals and says Type 2 patients often go into denial. They ignore advice and don’t take their medication. Guy’s and St Thomas’ vascular surgeon, Hany Zayed, is able to salvage many legs by bypassing a blockage or inserting a stent to keep blood flowing. But often, as the disease progresses, a blockage will occur again elsewhere. Often it’s a leg or a life, he says. For Zayed, an amputation is a failure. The key to surviving diabetes, he says, is “taking ownership of your health”. But most of his patients don’t look after themselves. Worse still, they ignore a foot infection after they’ve lost all feeling. Diabetics must check their feet daily, not walk barefoot, avoid ill-fitting shoes and get someone to cut their toenails. Zayed hates performing amputations. “It’s awful,” he says. “I have been trained for 20 years to save lives and legs.” http://www.mirror.co.uk/lifestyle/health/obesity-crisis-fuelling-rise-amputations-8083485 An impressive lecture about cannabis but with several references to cannabidiol and dietary modulators of the endocannabinoid system. He briefly discusses his 2004 theory of ECS dysfunction causing disease and provides evidence of ECS connection to common painful connections. Of special interest are pre & pro-biotics and foods shown to be effective in disease conditions and modulating the ECS. Many more lectures in this recent series. He also offers to share his information without restrictions including his upcoming comprehensive cannabis review article.. |




 RSS Feed
RSS Feed
