|
When Wendy Pogozelski began studying the primary literature in the field of nutrition, she was shocked to find enormous differences between the nutrition advice she’d found in the mainstream vs. the research and clinical results she was reading about. She connected with other researchers, doctors, biochemists and professors who had similar concerns and has become part of an international effort to help students, consumers and patients understand the science behind nutrition. Dr. Wendy Pogozelski received her B.S. in Chemistry from Chatham University and her PhD from The John Hopkins University. She was an Office of Naval Research post-doctoral fellow at the Naval Research Lab in Washington, D.C. In 1996, she came to Geneseo where she now holds the rank of Distinguished Teaching Professor and serves as Chair of the Chemistry Department. In her laboratory work, Dr. Pogozelski and her students investigate the effects of radiation on mitochondria. Since developing an interest in the biochemistry of nutrition, Dr. Pogozelski has been working with an international group of scientists and clinicians who are trying to bridge the gulf between scientific research and nutrition education.
0 Comments
Think about this, what kind of pressure are we exerting on our health each and every day? What is the effect of the food choices we make... or don’t make? Nick Murphy, owner of Mission Fitness, is a Certified Personal Trainer and Life Coach. He has 20+ years of experience in his field and is equipped to train clients across the fitness spectrum from the world-class athlete to the morbidly obese, and everyone in between. His passion is to teach people about health, fitness, diet and exercise, and to empower clients to take control of their lives.  I recently wrote a couple of posts explaining that over the years, I’ve revised my explanation of “the alternative hypothesis” from this: More Carbohydrates => Higher Insulin => Fat Storage to this: Damaging Diet => Hormonal Disruption => Fat Storage It’s not the biologically beneficial rise in insulin after a meal that makes people obese, I said in those posts. It’s chronically high insulin (along with other hormonal disruptions) resulting from a bad diet. In comments, a few of you suggested I read Dr. Jason Fung’s book The Obesity Code because it expresses similar ideas. Good suggestion. It’s an enlightening and very readable book – meaning it passes my “Aunt Martha” test. Your Aunt Martha could read this book without giving up because she doesn’t want to keep a medical dictionary on her desk. As I expected, insulin is still front and center in Fung’s explanation of why we get fat. In fact, the book’s cover includes the subhead Why your body’s own insulin is the key to controlling your weight. After citing plenty of research to effectively dismiss the “it’s all about consuming too many calories” explanation of obesity in the early chapters, Fung begins chapter seven like this: I can make you fat. Actually I can make anyone fat. How? By prescribing insulin. It won’t matter that you have willpower, or that you exercise. It won’t matter what you choose to eat. It’s simply a matter of enough insulin and enough time. Wait … hasn’t Dr. Fung read on the internet that we mustn’t blame insulin because it’s actually a wunnerful, wunnerful appetite suppressant? Well, perhaps he has … but if so, I’m sure he laughed. He has years of clinical experience with the stuff, as he explains in the book’s introduction: I’ve often watched patients start insulin treatment for their diabetes, knowing that most will gain weight. “Doctor,” they say, “you’ve always told me to lose weight. But the insulin you gave me makes me gain so much weight. How is this helpful?” … Like many doctors, I believed that weight gain was caloric imbalance – eating too much and moving too little. But if that were so, why did the medication I prescribed – insulin – cause such relentless weight gain? Fung answers his own question in chapter seven: Everything about human metabolism, including the body set weight, is hormonally regulated. A critical physiological variable such as body fatness is not left up the vagaries of daily caloric intake and exercise. Instead, hormones precisely and tightly regulate body fat. We don’t consciously control our body weight any more than we control our heart rates, our basal metabolic rates, our body temperatures or our breathing. But it isn’t just about insulin. Fung includes chapters on cortisol (which triggers weight gain partly by raising insulin) and other hormones, such as leptin, that are involved in weight regulation. And insulin isn’t just about how many grams of carbohydrate we consume. As Fung writes in chapter nine: The carbohydrate-insulin hypothesis, the idea that carbohydrates cause weight gain because of insulin secretion, was not exactly wrong. Carbohydrate-rich foods certainly do increase insulin levels to a greater extent than the other macronutrients. High insulin certainly does lead to obesity. However, the hypothesis stands incomplete. There are many problems, with the paradox of the Asian rice eater being the most obvious. … Indeed, many primitive societies that ate mostly carbohydrates have low obesity rates. In 1989, Dr. Staffan Lindeberg studied the residents of Kitava, one of the Trobriand Isands in Papua New Guinea’s archipelago – one of the last places on Earth where people ate a largely traditional diet. Starchy vegetables, including yam, sweet potato, taro and cassava, made up the basis of their diet. It isn’t foods that raise insulin that make us fat, Fung explains in the following chapters. It’s foods that lead to insulin resistance. Once we become insulin resistant, the entire hormonal system goes out of whack. Fung spends the next few chapters describing the foods that likely make us insulin resistant (sugar being a primary culprit) and how insulin resistance makes us fat. Insulin resistance is largely about what we eat. But rolling back the effects – and perhaps preventing insulin resistance in the first place – is also about when we eat. That was the most useful message in the book for me, since I’ve already read rather a lot about the effects of foods. As Fung explains, insulin is supposed to rise after meals. But then it’s supposed to drop and stay low for several hours. Back when few Americans were overweight, that’s what happened — because we ate three meals per day, period. Now we add constant snacking into the mix. When I was shooting interviews for Fat Head, Dr. Eric Oliver, author of Fat Politics, said that while people like Morgan Spurlock want to blame obesity on restaurants for serving larger meals, the real problem seems to be how often we eat between meals. Fung explains why that’s such a problem: The balance between the fed state (insulin dominant) and the fasted state (insulin deficient) has been completely destroyed. We are now spending most of our time in the fed state. … We are taught to eat the moment we roll out of bed. We are taught to eat throughout the day and again just before we sleep. We spend up to 18 hours in the insulin-dominant state, with only six hours insulin-deficient. A lousy diet, of course, makes snacking irresistible. Refined carbs jack up your blood sugar, and your body responds by flooding your bloodstream with enough insulin to give you low blood sugar. If you work in an office, I’m sure you’ve seen exactly what Fung is describing. I see people eat their white-bread sandwiches at noon, and by 3:30 they’re back in the cafeteria, trying to decide if they should raise blood sugar with a candy bar, a bag of chips, or some microwaved popcorn. Fung describes this as the vicious cycle that leads to insulin resistance. When insulin is too high, too often, cells down-regulate their insulin receptors. Then the body cranks out more insulin to try to lower high blood sugar. Then we get fatter. And hungrier. And snack more often. Part of the cure is real food, and Fung devotes a good chunk of the book to the topic. But another part of the cure is to dial back insulin resistance through intermittent fasting. As you know, I’m a fan of the Wisdom of Crowds. Fung reminds the reader that in nearly all ancient cultures, periodic fasting was considered a boon to good health. It was part of their wisdom. In the final chapter, Fung lays out the why and the how of intermittent fasting. Here’s part of the why: To break the insulin-resistance cycle, we must have recurrent periods of very low insulin levels. But how can we induce our body into a temporary state of very low insulin levels? We know that eating the proper foods prevents high levels, but it won’t do much to lower them. Some foods are better than others; nonetheless, all foods increase insulin production. If all foods raise insulin, then the only way for us to lower it is to completely abstain from food. The answer we are looking for is, in a word, fasting. In the rest of chapter, Fung describes the hormonal effects of fasting and dispels the many myths about going without food … such as “it will depress your metabolism.” Interestingly, the research he cites here and in other chapters shows that while living on a low-calorie, low-fat diet will indeed slow down your metabolism, periodic fasting doesn’t. Apparently we’re built for it. Given that paleo man’s hunts weren’t already successful, that makes sense. Jimmy Moore and Dr. Fung are co-authoring a book titled Fasting Clarity that’s scheduled to be published later this year. I’m looking forward to reading the expanded version of this topic. Source: http://www.fathead-movie.com/index.php/2016/06/27/review-the-obesity-code/ There may be a valid rationale to use potassium citrate as a supplement for those who are interested in improving beta cell function (i.e. diabetes) and insulin sensitivity.
Although the sample size is small, the research method for “Effects of potassium citrate or potassium chloride in patients with combined glucose intolerance: A placebo-controlled pilot study”, seems to hold its own. Conen K. et al., conducted this double-blind, placebo-controlled study with 7 males and 4 females ages 47-63 years old who were glucose intolerant (an umbrella term for metabolic conditions which result in higher than normal blood glucose. Pre-diabetes, type 2 diabetes, impaired fasting glucose and impaired glucose tolerance is defined by the World Health Organization as a fasting blood sugar level of 6.0 mmol/l) and found that both systolic and diastolic blood pressure, beta cell function and insulin sensitivity were significantly and positively affected when given 90 meqs of potassium citrate when compared with potassium chloride. They concluded that the citrate anion (The first intermediate of the citric acid or Krebs cycle, it plays an important role for fatty acids and it acts as a carrier for acetyl-CoA, and then synthesis for fatty acids.) is responsible for the insulin-sensitizing and blood pressure lowering results. Yet potassium itself may be more than a viable piece of the diabetes/insulin resistance treatment puzzle. One’s own genetic mutations (KCNJ11 gene and KCNQ1 (specific to the Asian population) affect potassium channels that influence insulin secretion, http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3197792/. Potassium:
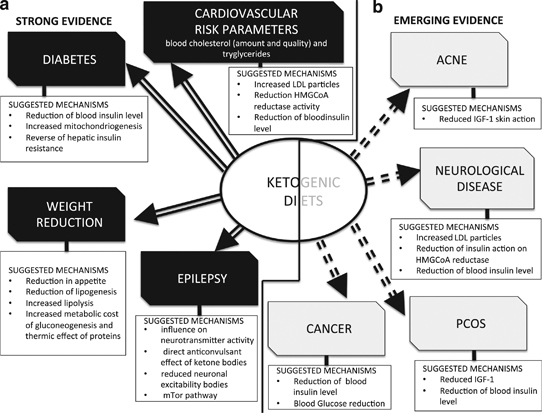
Potassium researchers recommend a diet that maintains an optimal sodium-to-potassium ratio of 1:5 or less, http://www.anaturalhealingcenter.com/documents/Thorne/monos/Potassium%20mono.pdf. Potassium recommendations for adolescents and adults is 4,700 mg/day, for children: 1 to 3 years of age is 3,000 mg/day, 4 to 8 years of age is 3,800 mg/day and 9 to 13 years of age is 4,500 mg/day. Foods that are good sources of potassium include: salmon, tuna, turkey, clams, avocado, white mushrooms, spinach, kale Swiss chard, collards, broccoli, blackberries, cantaloupe, grapefruit, artichokes and tomato. If you are not able to meet potassium recommendations, using a supplement seems prudent. There are certain population groups like the elderly, pregnant women or children, those with kidney issues, ulcers or anyone prone to metabolic alkalosis that should not use potassium supplements. Any nutrient supplementation should be supervised by a doctor. If potassium citrate can work as an insulin sensitizer while preserving beta cell function, it, along with other natural supplements like magnesium and chromium should be considered a first line option in diabetes treatment before using pharmaceutical drugs that have long lasting and more severe consequences. Source: https://valerieberkowitz.wordpress.com/2016/06/27/the-potassium-tie-in-to-insulin-sensitivity/ Introduction Ketosis is an often misunderstood subject. Its presence is thought to be equal to starvation or a warning sign of something going wrong in your metabolism. But nothing could be farther from the truth, except if you are an ill-treated type 1 diabetic person.[1] Ketones – contrary to popular belief and myth – are a much needed and essential healing energy source in our cells that come from the normal metabolism of fat. The entire body uses ketones in a more safe and effective way than the energy source coming from carbohydrates – sugar AKA glucose. Our bodies will produce ketones if we eat a diet devoid of carbs or a low carb diet (less than 60 grams of carbs per day).[2] By eating a very low carb diet or no carbs at all (like a caveman) we become keto-adapted. In fact, what is known today as the ketogenic diet was the number one treatment for epilepsy until Big Pharma arrived with its dangerous cocktails of anti-epileptic drugs. It took several decades before we heard again about this diet, thanks in part to a parent who demanded it for his 20-month-old boy with severe seizures. The boy’s father had to find out about the ketogenic diet in a library as it was never mentioned as an option by his neurologist. After only 4 days on the diet, his seizures stopped and never returned.[3] The Charlie Foundation was born after the kid’s name and his successful recovery, but nowadays the ketogenic diet is available to the entire world and it’s spreading by word of mouth thanks to its healing effects. It is not only used as a healthy lifestyle, it is also used for conditions such as infantile spasms, epilepsy, autism, brain tumors, Alzheimer’s disease, Lou Gehrig’s disease, depression, stroke, head trauma, Parkinson’s disease, migraine, sleep disorders, schizophrenia, anxiety, ADHD, irritability, polycystic ovarian disease, irritable bowel syndrome, gastroesophageal reflux, obesity, cardiovascular disease, acne, type 2 diabetes, tremors, respiratory failure and virtually every neurological problem but also cancer, and conditions where tissues need to recover after a loss of oxygen.[4] Our body organs and tissues work much better when they use ketones as a source of fuel, including the brain, heart and the core of our kidneys. If you ever had a chance to see a heart working in real time, you might have noticed the thick fatty tissue that surrounds it. In fact, heart surgeons get to see this every day. A happy beating heart is one that is surrounded by layers of healthy fat. Both the heart and the brain run at least 25% more efficiently on ketones than on blood sugar. Ketones are the ideal fuel for our bodies unlike glucose – which is damaging, less stable, more excitatory and in fact shortens your life span. Ketones are non-glycating, which is to say, they don’t have a caramelizing ageing effect on your body. A healthy ketosis also helps starve cancer cells as they are unable to use ketones for fuel, relying on glucose alone for their growth. [5]The energy producing factories of our cells – the mitochondria – work much better on a ketogenic diet as they are able to increase energy levels in a stable, long-burning, efficient, and steady way. Not only that, a ketogenic diet induces epigenetic changes[6] which increases the energetic output of our mitochondria, reduces the production of damaging free radicals, and favours the production of GABA – a major inhibitory brain chemical. GABA has an essential relaxing influence and its favored production by ketosis also reduces the toxic effects of excitatory pathways in our brains. Furthermore, recent data suggests that ketosis alleviates pain in addition to having an overall anti-inflammatory effect. [7] The ketogenic diet acts on multiple levels at once, something that no drug has been able to mimic. This is because mitochondria are specifically designed to use fat for energy. When our mitochondria use fat as an energetic source, its toxic load is decreased, the expression of energy producing genes are increased, its energetic output is increased, and the load of inflammatory energetic-end-products is decreased. The key of these miraculous healing effects relies on the fact that fat metabolism and its generation of ketone bodies (beta-hydroxybutyrate and acetoacetate) by the liver can only occur within the mitochondrion, leaving chemicals within the cell but outside the mitochondria readily available to stimulate powerful anti-inflammatory antioxidants. The status of our mitochondria is the ultimate key for optimal health and while it is true that some of us might need extra support in the form of nutritional supplementation to heal these much needed energy factories, the diet still remains the ultimate key for a proper balance. Our modern world’s staple energetic source is sugar which needs to be processed first in the cell soup before it can be passed into the energy factory of the cell- the mitochondrion. Energy sources from fat don’t require this processing; it goes directly into the mitochondria for energetic uses. That is, it is more complicated to create energy out of sugar than out of fat. As Christian B. Allan, PhD and Wolfgang Lutz, MD said in their book Life Without Bread: Carbohydrates are not required to obtain energy. Fat supplies more energy than a comparable amount of carbohydrate, and low-carbohydrate diets tend to make your system of producing energy more efficient. Furthermore, many organs prefer fat for energy.The fact is you get MORE energy per molecule of fat than sugar. How many chronic and autoimmune diseases have an energy deficit component? How about chronic fatigue? Fibromyalgia? Rheumatoid Arthritis? Multiple Sclerosis? Cancer? Back to Allan and Lutz: Mitochondria are the power plants of the cell. Because they produce most of the energy in the body, the amount of energy available is based on how well the mitochondria are working. Whenever you think of energy, think of all those mitochondria churning out ATP to make the entire body function correctly. The amount of mitochondria in each cell varies, but up to 50 percent of the total cell volume can be mitochondria. When you get tired, don’t just assume you need more carbohydrates; instead, think in terms of how you can maximize your mitochondrial energy production…If you could shrink to a small enough size to get inside the mitochondria, what would you discover? The first thing you’d learn is that the mitochondria are primarily designed to use fat for energy! In short, let fat be thy medicine and medicine be thy fat! You will think that with all of this information we would see ketogenic diets recommended right and left by our health care providers, but alas, that is not the case. Mainstream nutritionists recommend carbohydrates AKA sugar as the main staple of our diets. The problem with this (and there are several of them) is that in the presence of a high carb diet we are unable to produce ketones from the metabolism of fats, thus, depriving our bodies from much healing ketone production. The fact that we live in a world which uses glucose as a primary fuel means that we eat a very non healing food in more ways than one. I have been doing the low carb diet for about a week and a half now and I must say, I am really starting to feel amazing!!! The first few days my head hurt, I felt lethargic, and my legs felt so heavy. But after I got past that, I have so much energy. I don’t get tired anymore around 3pm. The best part is, I am not constantly thinking and obsessing about food. I feel a real sense of inner calm. My skin looks better, my hair looks better too. I have been having bacon and eggs for breakfast, a pork chop or other piece of meat for lunch, and usually some pork and sometimes some green beans for dinner. I have also lost some weight! Woo hoo!!! -Angela, United States. Sott.net forum. We have been on a ketogenic diet for nearly three million years and it has made us human. It was the lifestyle in which our brains got nurtured and evolved. But not anymore, unless we all make an effort to reclaim this lost wisdom. Nowadays the human brain is not only shrinking, but brain atrophy is the norm as we age and get plagued with diseases such as Alzheimer’s disease, Parkinson’s disease, senile dementia and so forth. In the mean time new research is starting to elucidate the key role of our mitochondria in the regulation of the cell cycle – the vital process by which a single celled fertilized egg develops into a mature organism, as well as the process by which hair, skin, blood cells, and some internal organs are renewed. In the complicated and highly choreographed events surrounding cell-cycle progression, mitochondria are not simple bystanders merely producing energy but instead are full-fledged participants.[8] Given the significant amount of energy needed to make all the nutrients required for cell division, it makes sense that some coordination existed. This long ignored and overlooked connection between the mitochondria and the cell cycle is something that is worthy of considerably more attention as we understand the role of diet in our bodies. We’ll have to take a closer look at this subject of ketosis, as it really holds the key to unlock our transformational pathways that will lead us to an outstanding healthy living. Mitochondrial Dysfunction Mitochondria are best known as the powerhouses of our cells since they produce the cell’s energy. But they also lead the genetic orchestra which regulates how every cell ages, divides, and dies. They help dictate which genes are switched on or off in every single cell of our organism. They also provide the fuel needed to make new brain connections, repair and regenerate our bodies. Whether we are housewives, sportsmen or labourers, energy is a topic that concerns us all, every day and in every way. Our well being, behaviour and ability to perform the tasks put in front of us is all to do with our individual levels of energy. But how do we derive energy from the foods that we eat? There are many man-made myths surrounding energy production in the body and which foods supply energy. Mainstream science says that carbohydrates are what mitochondria use as fuel for energy production. This process is called oxidative metabolism because oxygen is consumed in the process. The energy produced by mitochondria is stored in a chemical “battery”, a unique molecule called adenosine triphosphate (ATP). Energy-packed ATP can then be transported throughout the cell, releasing energy on demand of specific enzymes. In addition to the fuel they produce, mitochondria also create a by-product related to oxygen called reactive oxygen species (ROS), commonly known as free radicals. But what we are not told is that mitochondria were specifically designed to use fat for energy, not carbohydrate. Source: Christian B. Allan, PhD and Wolfgang Lutz, MD, Life Without Bread. There are several very complicated steps in making ATP within mitochondria, but a look at 5 major parts of ATP production will be all that you need to know in order to understand how energy is created within our mitochondria and why fats are the key to optimize their function. Don’t get focused on specific names, just try to see the whole picture. Step 1 – Transportation of Food-Based Fuel Source into the Mitochondria Fuel must first get into the mitochondria where all the action happens. Fuel can come from carbs or it can come from fats. Fatty acids are the chemical name for fat, and medium and large sized fatty acids get into the mitochondria completely intact with the help of L-carnitine. Think of L-carnitine as a subway train that transports fatty acids into the mitochondria. L-carnitine (from the Greek word carnis means meat or flesh) is chiefly found in animal products. Fuel coming from carbs needs to get broken down first outside the mitochondria and the product of this breakdown (pyruvate) is the part that gets transported inside the mitochondria, or it can be used to produce energy in a very inefficient way outside the mitochondria through anaerobic metabolism which produces ATP when oxygen is not present. Step 2 – Fuel is Converted into Acetyl-CoA When pyruvate – the product of breaking down carbs – enters the mitochondria, it first must be converted into acetyl-CoA by an enzymatic reaction. Fatty acids that are already inside the mitochondria are broken down directly into acetyl-CoA in what is called beta-oxidation. Acetyl-CoA is the starting point of the next step in the production of ATP inside the mitochondria. Step 3 – Oxidation of Acetyl-CoA and the Krebs Cycle The Krebs cycle (AKA tricarboxylic acid cycle or citric acid cycle) is the one that oxidizes the acetyl-CoA, removing thus electrons from acetyl-CoA and producing carbon dioxide as a by-product in the presence of oxygen inside the mitochondria. Step 4 – Electrons Are Transported Through the Respiratory Chain The electrons obtained from acetyl-CoA – which ultimately came from carbs or fats – are shuttled through many molecules as part of the electron transport chain inside the mitochondria. Some molecules are proteins, others are cofactors molecules. One of these cofactors is an important substance found mainly in animal foods and it is called coenzyme Q-10. Without it, mitochondrial energy production would be minimal. This is the same coenzyme Q10 that statins drug block producing crippling effects on people’s health. Step 4 is also where water is produced when oxygen accepts the electrons. Step 5 – Oxidative phosphorylation As electrons travel down the electron transport chain, they cause electrical fluctuations (or chemical gradients) between the inner and outer membrane in the mitochondria. These chemical gradients are the driving forces that produce ATP in what is called oxidative phosphorylation. Then the ATP is transported outside the mitochondria for the cell to use as energy for any of its thousands of biochemical reactions. But why is fat better than carbs? If there were no mitochondria, then fat metabolism for energy would be limited and not very efficient. But nature provided us during our evolution with mitochondria that specifically uses fat for energy. Fat is the fuel that animals use to travel great distances, hunt, work, and play since fat gives more energy-packed ATPs than carbs. Biochemically, it makes sense that if we are higher mammals who have mitochondria, then we need to eat fat. Whereas carb metabolism yields 36 ATP molecules from a glucose molecule, a fat metabolism yields 48 ATP molecules from a fatty acid molecule inside the mitochondria. Fat supplies more energy for the same amount of food compared to carbs. But not only that, the burning of fat by the mitochondria – beta oxidation – produces ketone bodies that stabilizes overexcitation and oxidative stress in the brain related to all its diseases, it also causes epigenetic changes that produce healthy and energetic mitochondria and decreasing the overproduction of damaging and inflammatory free radicals among many other things! Mitochondria regulate cellular suicide, AKA apoptosis, so that old and dysfunctional cells which need to die will do so, leaving space for new ones to come into the scene. But when mitochondria function becomes impaired and sends signals that tell normal cells to die, things go wrong. For instance, the destruction of brain cells leads to every single neurodegenerative condition known including Alzheimer’s disease, Parkinson’s disease and so forth. Mitochondrial dysfunction has wide-ranging implications, as the health of the mitochondria intimately affects every single cell, tissue and organ within your body. The catalysts for this destruction is usually uncontrolled free radical production which causes oxidative damage to tissues, fat, proteins, DNA; causing them to rust. This damage, called oxidative stress, is at the basis of oxidized cholesterol, stiff arteries (rusty pipes) and brain damage. Oxidative stress is a key player in dementia as well as autism. We produce our own anti-oxidants to keep a check on free radical production, but these systems are easily overwhelmed by a toxic environment and a high carb diet, in other words, by today’s lifestyle and diet. Mitochondria also have interesting characteristics which differentiate them from all other structural parts of our cells. For instance, they have their own DNA (referred as mtDNA) which is separate from the widely known DNA in the nucleus (referred as n-DNA). Mitochondrial DNA comes for the most part from the mother line, which is why mitochondria is also considered as your feminine life force. This mtDNA is arranged in a ring configuration and it lacks a protective protein surrounding, leaving its genetic code vulnerable to free radical damage. If you don’t eat enough animal fats, you can’t build a functional mitochondrial membrane which will keep it healthy and prevent them from dying. If you have any kind of inflammation from anywhere in your body, you damage your mitochondria. The loss of function or death of mitochondria is present in pretty much every disease. Dietary and environmental factors lead to oxidative stress and thus to mitochondrial injury as the final common pathway of diseases or illnesses. Autism, ADHD, Parkinson’s, depression, anxiety, bipolar disease, brain ageing are all linked with mitochondrial dysfunction from oxidative stress. Mitochondrial dysfunction contributes to congestive heart failure, type 2 diabetes, autoimmune disorders, ageing, cancer, and other diseases. Whereas the nDNA provides the information your cells need to code for proteins that control metabolism, repair, and structural integrity of your body, it is the mtDNA which directs the production and utilization of your life energy. A cell can still commit suicide (apoptosis) even when it has no nucleus nor nDNA. Because of their energetic role, the cells of tissues and organs which require more energy to function are richer in mitochondrial numbers. Cells in our brains, muscles, heart, kidney and liver contain thousands of mitochondria, comprising up to 40% of the cell’s mass. According to Prof. Enzo Nisoli, a human adult possesses more than ten million billion mitochondria, making up a full 10% of the total body weight.[9] Each cell contains hundreds of mitochondria and thousands of mtDNA. Since mtDNA is less protected than nDNA because it has no “protein” coating (histones), it is exquisitely vulnerable to injury by destabilizing molecules such as neurotoxic pesticides, herbicides, excitotoxins, heavy metals and volatile chemicals among others. This increasees free radical production to the extreme which then leads to oxidative stress damaging our mitochondria and its DNA. As a result we get overexcitation of cells and inflammation which is at the root of Parkinson’s disease and other diseases, but also mood problems and behaviour problems. Enough energy means a happy and healthy life. It also reflects in our brains with focused and sharp thinking. Lack of energy means mood problems, dementia, and slowed mental function among others. Mitochondria are intricately linked to the ability of the prefrontal cortex –our brain’s captain- to come fully online. Brain cells are loaded in mitochondria that produce the necessary energy to learn and memorize, and fire neurons harmoniously. The sirtuin family of genes works by protecting and improving the health and function of your mitochondria.[10] They are positively influenced by a diet that is non-glycating, i.e. a low carb diet as opposed to a high carb diet which induces mitochondrial dysfunction and formation of reactive oxygen species. Another thing that contributes to mitochondrial dysfunction is latent viral infection such as the ones of the herpes family. As I mentioned in On Viral “Junk” DNA, a DNA Enhancing Ketogenic Diet, and Cometary Kicks, most, if not all of your “junk” DNA has viral-like properties. If a pathogenic virus takes hold of our DNA or RNA, it could lead to disease or cancer. Herpes simplex virus is a widespread human pathogen and it goes right after our mitochondrial DNA. Herpes simplex virus establishes its latency in sensory neurons, a type of cell that is highly sensitive to the pathological effects of mt DNA damage.[11] A latent viral infection might be driving the brain cell loss in neurodegenerative diseases such as Alzheimer’s disease.[12]As I speculated in Heart attacks, CFS, herpes virus infection and the vagus nerve , a latent herpes virus infection might drive more diseases than we would like to admit. Members of the herpes virus family (i.e. cytomegalovirus and Epstein-Barr virus which most people have as latent infections!), can go after our mitochondrial DNA, causing neurodegenerative diseases by mitochondrial dysfunction. But a ketogenic diet is the one thing that would help stabilize mtDNA since mitochondria runs the best on fat fuel. As it happens, Alzheimer’s disease is the one condition where a ketogenic diet has its most potential healing effect.[4] The role of mitochondrial dysfunction in our “modern” age maladies is a staggering one. Optimal energetic sources are essential if we are to heal from chronic ailments. It is our mitochondria which lies at the interface between the fuel from foods that come from our environment and our bodies’ energy demands. And it is a metabolism based on fat fuel, a ketone metabolism, the one which signals epigenetic changes that maximizes energetic output within our mitochondria and help us heal. I am incredulous at how my body is responding. I think I am totally carb intolerant. I’ve struggled with extreme fatigue/exhaustion for so many years, even with improved sleep in a dark room that I can’t tell you how wonderful it is to wake up in the morning, get out of bed and not long to crawl back in, going through the day by will mostly. Also chronic long-standing intestinal issues are finally resolving. A couple of people at work have made comments to the effect that I’m a “different woman”, calmer, no more 'hyperness' under pressure, stress seems to roll off of my back as well. I’ve lost a little weight and although I don’t weigh myself, my clothes are definitely looser. I’ve had the round middle for so many years I was resigned to struggling to bend over to pull my shoes on! -Bluefyre, 56 years old, United States. Sott.net forum Ketosis – Closer Look The presence of ketones in the blood and urine, a condition known as ketosis, has always been regarded as a negative situation, related to starvation. While it is true that ketones are produced during fasting, ketones are also produced in times of plenty, but not plenty of carbohydrates since a carb metabolism suppresses ketosis. In the absence of most carbs in the diet, ketones will form from fat to supply energy. This is true even if lots of fats and enough protein are eaten, something that is hardly a starvation condition. As we already saw, a ketogenic diet has been proved useful in a number of diseases, especially neurological ones. Strictly speaking, a ketogenic diet is a high fat diet in which carbohydrates are either completely eliminated or nearly eliminated so that the body has the very bare minimum sources of glucose. That makes fats (fatty acids) a mandatory energetic fuel source for both the brain and other organs and tissues. If your carb intake is high, you’ll end up storing both the fat and the carbs in your fat tissue thanks to the hormone insulin. A ketogenic diet is not a high protein diet, which as it happens, can also stimulate insulin. It is basically a diet where you rely primarily on animal foods and especially their fats. I recently had my annual blood work done (cholesterol, etc.) During the review, my doctor said that everything looked great! He then encouraged me to continue on my great ‘low fat, high fruit and veggie diet’ that I must be following! I just smiled. Next visit I’m going to tell him about my real ‘diet’. Lol -1984, United States. Sott.net forum. Among the by-products of fat burning metabolism are the so called ketone bodies – acetoacetate, β-hydroxybutyrate and acetone – which are produced for the most part by the liver. When our bodies are running primarily on fats, large amounts of acetyl-CoA are produced which exceed the capacity of the Krebs cycle, leading to the making of these three ketone bodies within liver mitochondria. Our levels of ketone bodies in our blood go up and the brain readily uses them for energetic purposes. Ketone bodies cross the blood brain barrier very readily. Their solubility also makes them easily transportable by the blood to other organs and tissues. When ketone bodies are used as energy, they release acetyl-CoA which then goes to the Krebs cycle again to produce energy. In children who were treated with the ketogenic diet to treat their epilepsy, it was seen that they become seizure-free even long after the diet ended, meaning that not only did the diet proved to be protective, but also it modified the activity of the disease , something that no drug has been able to do.[13] In Alzheimer’s disease, as levels of ketone bodies rise, memory improves. People’s starved brains finally receive the much needed fats they need! In fact, every single neurological disease is improved on the ketogenic diet. The benefits of a ketogenic diet can be seen as quickly as one week, developing gradually over a period of 3 weeks. There are several changes in gene expression involving metabolism, growth, development, and homeostasis among others. The hippocampus is a region in your brain that is very vulnerable to stress which makes it lose its brain cells. The hippocampus has to do with memory, learning, and emotion. As it happens, a ketogenic diet promotes the codification of genes which creates mitochondria in the hippocampus, making more energy available. A larger mitochondrial load and more energy means more reserve to withstand much more stress.[14] In some animal models, following a ketogenic diet, there is a 50% increase in the total number of mitochondria in the hippocampus, resulting in more brain ATP.[15] Other animal studies show how communication between brain cells in the hippocampus would remain smooth for 60% longer when exposed to a stressful stimulus compared to their counterparts who didn’t had a ketogenic diet.[16] This is very important since too much stress can damage the hippocampus and its capacity to retrieve information, making you “absent-minded” or “brain-scattered”, as well as affecting the ability of your prefrontal cortex to think and manage behavior. A ketogenic diet also increases levels of the calming neurotransmitter – GABA - which then serves to calm down the overexcitation which is at the base of major neuro-degenerative diseases, but also anxiety and other mood problems. A ketogenic diet also increases antioxidant pathways that level the excess production of free radicals from a toxic environment. It also enhances anti-inflammatory pathways. Ketosis also cleans our cells from proteins that act like “debris” and which contribute to ageing by disrupting a proper functioning of the cell.[17] It basically does this by what is known as autophagy which preserves the health of cells and tissues by replacing outdated and damaged cellular components with fresh ones. This prevents degenerative diseases, ageing, cancer, and protects you against microbial infections. A ketogenic diet not only rejuvenates you, it also makes a person much less susceptible to viruses and bacterial infections.[18] This is very relevant due to the increasing number of weird viral and bacterial infections that seem to be incoming from our upper atmosphere[19] (for more information see New Light on the Black Death: The Viral and Cosmic Connection), or due to high levels of radiation that creates more pathogenic strains (see Detoxify or Die: Natural Radiation Protection Therapies for Coping With the Fallout of the Fukushima Nuclear Meltdown). Either way, we are more vulnerable than ever due to the state of our mitochondria. But we can prepare for the worst with ketosis. Ketone-enhanced autophagy is very important because autophagy can target viruses and bacteria that grow inside cells which are very problematical.[20] Intracellular viruses and bacteria can lead to severe mitochondrial dysfunction and ketosis remains by far our best chance against them. A Paoli, A Rubini, J S Volek and K A Grimaldi. Beyond weight loss: a review of the therapeutic uses of very-low-carbohydrate (ketogenic) diets. European Journal of Clinical Nutrition (2013) 67, 789–796 Ketone bodies production through intermittent fasting and the ketogenic diet is the most promising treatment for mitochondrial dysfunction.[21]The longevity benefits seen by caloric restriction research is due to the fact that our bodies shift to a fat burning metabolism within our mitochondria. With a ketogenic diet, we go into a fat burning metabolism without restricting our caloric intake.
Ketosis deals effectively with all the problems of a diet rich in carbs – the one recommended by mainstream science. Namely a ketogenic diet deals with anxiety, food cravings, irritability, tremors, and mood problems among others. It is a crime to discourage the consumption of a high fat diet considering that a ketogenic diet shrinks tumours in human and animal models, and enhances our brain’s resilience against stress and toxicity. In addition to increasing the production of our body’s natural valium – GABA – the increased production of acetyl-CoA generated from the ketone bodies also drives the Krebs cycle to increase mitochondrial NADH (reduced nicotinamide adenine nucleotide) which our body uses in over 450 vital biochemical reactions – including the cell signalling and assisting of the ongoing DNA repair. Because the ketone body beta-hydroxybutyrate is more energy rich than pyruvate, it produces more ATP. Ketosis also enhances the production of important anti-oxidants that deal with toxic elements from our environments, including glutathione. Mitochondria from the hippocampus of ketogenic diet-fed animals are also resistant to mtDNA damage and are much less likely to commit cell suicide –apoptosis- at inappropriate times. As Douglas C. Wallace, PhD, Director of the Center for Mitochondrial and Epigenomic Medicine says, “the ketogenic diet may act at multiple levels: It may decrease excitatory neuronal activity, increase the expression of bioenergetic genes, increase mitochondrial biogenesis and oxidative energy production, and increase mitochondrial NADPH production, thus decreasing mitochondrial oxidative stress.”[21] Keto-adaptation results in marked changes in how we construct and maintain optimum membrane (“mem-brain”) composition, not only because of the healthy fats we provide through the diet, but also because of less free radical production and inflammatory mediators, along with more production of anti-oxidants. It is really the ideal balanced state. Moreover, you might want to keep in mind this excerpt from "Human Brain Evolution: The Influence of Freshwater and Marine Food Resources"[22]: There are two key advantages to having ketone bodies as the main alternative fuel to glucose for the human brain. First, humans normally have significant body fat stores, so there is an abundant supply of fatty acids to make ketones. Second, using ketones to meet part of the brain’s energy requirement when food availability is intermittent frees up some glucose for other uses and greatly reduces both the risk of detrimental muscle breakdown during glucose synthesis, as well as compromised function of other cells dependent on glucose, that is, red blood cells. One interesting attribute of ketone uptake by the brain is that it is four to five times faster in newborns and infants than in adults. Hence, in a sense, the efficient use of ketones by the infant brain means that it arguably has a better fuel reserve than the adult brain. Although the role of ketones as a fuel reserve is important, in infants, they are more than just a reserve brain fuel – they are also the main substrate for brain lipid synthesis. I have hypothesized that evolution of a greater capacity to make ketones coevolved with human brain expansion. This increasing capacity was directly linked to evolving fatty acid reserves in body fat stores during fetal and neonatal development. To both expand brain size and increase its sophistication so remarkably would have required a reliable and copious energy supply for a very long period of time, probably at least a million, if not two million, years. Initially, and up to a point, the energy needs of a somewhat larger hominin brain could be met by glucose and short – term glucose reserves such as glycogen and glucose synthesis from amino acids. As hominins slowly began to evolve larger brains after having acquired a more secure and abundant food supply, further brain expansion would have depended on evolving significant fat stores and having reliable and rapid access to the fuel in those fat stores. Fat stores were necessary but were still not sufficient without a coincident increase in the capacity for ketogenesis. This unique combination of outstanding fuel store in body fat as well as rapid and abundant availability of ketones as a brain fuel that could seamlessly replace glucose was the key fuel reserve for expanding the hominin brain, a reserve that was apparently not available to other land – based mammals, including nonhuman primates.It is indisputable that a ketogenic diet has protective effects in our brains. With all the evidence of its efficacy in mitochondrial dysfunction, it can be applied for all of us living in a highly stressful and toxic environment. Ketone bodies are healing bodies that helped us evolve and nowadays our mitochondria are always busted in some way or another since the odds in this toxic world are against us. Obviously, there are going to be people with such damaged mtDNA or with mutations they were born with, who can’t modify their systems (i.e. defects on L-carnitine metabolism), but even in some of those cases, they can halt or slow down further damage. Our healthy ancestors never had to deal with the levels of toxicity that we live nowadays and nevertheless, they ate optimally. Considering our current time and environment, the least we can do is eat optimally for our physiology. The way to have healing ketone bodies circulating in our blood stream is to do a high fat, restricted carb and moderated protein diet. Coupled with intermittent fasting which will enhance the production of ketone bodies, and resistance training which will create mitochondria with healthier mtDNA, we can beat the odds against us. What is considered nowadays a “normal diet” is actually an aberration based on the corruption of science which benefits Big Agra and Big Pharma. If we would go back in time to the days before the modern diet became normalized by corporative and agricultural interests, we will find that ketosis was the normal metabolic state. Today’s human metabolic state is aberrant. It is time to change that. References[1] A research member of sott.net’s forum has diabetes type 1 and is doing the ketogenic diet. Under normal circumstances, diabetics (including type I) report amazing results on a low-carbohydrate diet. See Dr. Bernstein’s Diabetics Solution by Richard K. Bernstein, MD (Little, Brown and Company: 2007). [2] It varies among each person, but the general range is between 0 and 70 grams of carbs plus moderate intake of protein, between 0.8 and 1.5 grams of protein per kg of ideal body weight. Pregnant women and children should not have their protein restricted. [3] Ketogenic diets in seizure control and neurologic disorders by Eric Kossoff, MD, Johns Hopkins Hospital, Baltimore, Maryland. The Art and Science of Low Carbohydrate Living by Jeff S. Volek, PhD, Rd and Stephen D. Phinney, MD, PhD. Beyond Obesity, LLC , 2011. [4] A Paoli, A Rubini, J S Volek and K A Grimaldi. Beyond weight loss: a review of the therapeutic uses of very-low-carbohydrate (ketogenic) diets. European Journal of Clinical Nutrition (2013) 67, 789–796 [5] Rainer J Klement, Ulrike Kämmerer. Is there a role for carbohydrate restriction in the treatment and prevention of cancer? Nutr Metab (Lond). Oct 26, 2011; 8: 75. [6] If the genetic code is the hardware for life, the epigenetic code is software that determines how the hardware behaves. [7] David N. Ruskin and Susan A. Masino, The Nervous System and Metabolic Dysregulation: Emerging Evidence Converges on Ketogenic Diet Therapy. Front Neurosci. 2012; 6: 33. [8] Finkel T, Hwang PM. The Krebs cycle meets the cell cycle: mitochondria and the G1-S transition. Proc Natl Acad Sci U S A. 2009 Jul 21;106(29):11825-6. [9] Matthews C.M. Nurturing your divine feminine. Proc (Bayl Univ Med Cent). 2011 July; 24(3): 248. [10] Hipkiss AR. Energy metabolism, altered proteins, sirtuins and ageing: converging mechanisms? Biogerontology. 2008 Feb;9(1):49-55. [11] Saffran HA, Pare JM, Corcoran JA, et al. Herpes simplex virus eliminates host mitochondrial DNA. EMBO Rep. 2007 Feb;8(2):188-93. [12] Porcellini E, Carbone I, et al. Alzheimer’s disease gene signature says: beware of brain viral infections. Immun Ageing. 2010 Dec 14;7:16. [13] Gasior M, Rogawski MA, Hartman AL. Neuroprotective and disease-modifying effects of the ketogenic diet. Behav Pharmacol. 2006 Sep;17(5-6):431-9. [14] Maalouf M, Rho JM, Mattson MP. The neuroprotective properties of calorie restriction, the ketogenic diet, and ketone bodies. Brain Res Rev. 2009 Mar;59(2):293-315. [15] Nylen K, Velazquez JL. The effects of a ketogenic diet on ATP concentrations and the number of hippocampal mitochondria in Aldh5a1(-/-) mice. Biochim Biophys Acta. 2009 Mar;1790(3):208-12. [16] Bough K. Energy metabolism as part of the anticonvulsant mechanism of the ketogenic diet. Epilepsia. 2008 Nov;49 Suppl 8:91-3. [17] Finn PF, Dice JF. Ketone bodies stimulate chaperone-mediated autophagy. J Biol Chem. 2005 Jul 8;280(27):25864-70. [18] Yuk JM, Yoshimori T, Jo EK. Autophagy and bacterial infectious diseases. Exp Mol Med. 2012 Feb 29;44(2):99-108. [19] Chandra Wickramasinghe, Milton Wainwright & Jayant Narlika. SARS – a clue to its origins? The Lancet, vol. 361, May 23, 2003, pp 1832. [20] Yordy B, Iwasaki A. Autophagy in the control and pathogenesis of viral infection. Curr Opin Virol. 2011 Sep;1(3):196-203. [21] Douglas C. Wallace, Weiwei Fan, and Vincent Procaccio. Mitochondrial Energetics and Therapeutics Annu Rev Pathol. 2010; 5: 297–348. [22] Stephen Cunnane, Kathlyn Stewart.Human Brain Evolution: The Influence of Freshwater and Marine Food Resources. June 2010, Wiley-Blackwell. Gabriela Segura, MD Friday, 9 August 2013 Source: http://www.drmyhill.co.uk/wiki/Ketogenic_diet_-_a_connection_between_mitochondria_and_diet  Some medical professionals confuse ketoacidosis, an extremely abnormal form of ketosis, with the normal benign ketosis associated with ketogenic diets and fasting states in the body. They will then tell you that ketosis is dangerous. Ketosis is NOT Ketoacidosis The difference between the two conditions is a matter of volume and flow rate*: *See this reference paper.
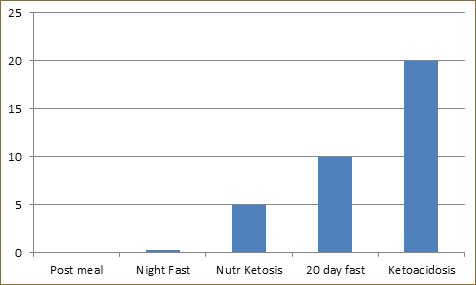
Body Condition Quantity of Ketones Being Produced After a meal: 0.1 mmol/L Overnight Fast: 0.3 mmol/L Ketogenic Diet (Nutritional ketosis): 1-8 mmol/L >20 Days Fasting: 10 mmol/L Uncontrolled Diabetes (Ketoacidosis): >20 mmol/LHere's a more detailed explanation: Fact 1: Every human body maintains the blood and cellular fluids within a very narrow range between being too acidic (low pH) and too basic (high pH). If the blood pH gets out of the normal range, either too low or too high, big problems happen. Fact 2: The human pancreas is an organ which secretes insulin, a hormone that helps the body manage blood sugar and fat storage. Without insulin, the body cannot utilize glucose for fuel in the cells, AND cannot store fat in the fat cells. This is why one of the symptoms of Type 1 diabetes is unexplained weight loss. Type 1 diabetics have pancreatic damage which results in a complete lack of insulin production, and as a consequence, their fat cells have no insulin message telling them to "hold on to those fatty acids". Without that message from insulin, large quantities of fatty acids flow out of the fat cells and are broken down in the liver into a ketone body called acetoacetic acid which is then converted to two other circulation ketone bodies, beta-hydroxybutyrate and acetone. This is ketosis, but an unrestrained, abnormally excessive ketosis. The danger is in the amount of ketone bodies being released. Because ketone bodies are slightly acidic in nature, and so many are released at once in a uncontrolled event, they build up in the bloodstream. The sheer volume quickly overwhelms the delicate acid-base buffering system of the blood, and the blood pH becomes more acidic than normal. A change in blood pH causes many unhealthy downstream effects. It is not the ketone bodies which are dangerous, it is the low blood pH, a condition called acidosis. Acidosis symptoms include fruity breath (from the acetone), nausea, hyperventilation, (deep, rapid breathing) dehydration and low blood pressure, as the body tries to rid itself of the abnormal amounts of ketones through the lungs and urine. If left untreated, acidosis can result in a coma and death. Treatment includes the administration of insulin to slow the ketosis and fluid replacement. Type 1 diabetics can develop diabetic ketoacidosis if they don't inject enough insulin, and this usually occurs during a period of illness or injury, or may be the precipitating condition which results in the diagnosis of their disease. Ketogenic acidosis can also happen during:
Nutrional ketosis associated with a properly formulated ketogenic diet is not dangerous because it is regulated by insulin within the body. It's simply the metabolic process of burning your own body fat for fuel, and unless you are diabetic and lacking insulin, or you are a raging alcoholic, it is perfectly safe. Levels for adults with a working pancreas and insulin production rarely get above 8-10 mmol/L. Here's another explanation from Dr. Peter Attia, a physician with extensive knowledge about ketosis.  If your insulin resistant and eat a high carbohydrate (Glucose) meal this will create havoc with your metabolic system.1) You already have plenty of available glucose stored in your liver, your blood has excess glucose circulating that cannot enter your cells because of your level of insulin resistance. 2) You have Glut transporters that need to be brought to the surface of the cell to allow glucose entry into the cell. Insulin brings this Glut transporter to the cell surface. Because of your level of insulin resistance only a small portion of the glucose can enter the cells. The excess (leftover) glucose must be dealt with. 3) This excess glucose needs to be dealt with. Excess glucose is toxic to your cells and to the blood itself. This excess glucose is send to the liver. The liver is where fat production takes place. The liver converts this excess glucose to mainly saturated fat (C-16 Palmitic). 4) Fat like cholesterol does not mix with our water soluble blood. They both need to be bound to a carrier (Lipoprotein) for transport in the blood. 5) The human body has 2 distinct lipoprotein systems, one for dietary fat, one for liver made fat. 6) The lipoprotein made in the liver for the transport of this liver made fat is the lipoprotein VLDL, very low density lipoprotein. This lipoprotein VLDL key identifying protein is APOB100. 7) This VLDL eventually morphs into the small/dense Particle B lipoprotein. This causes most of your LDL cholesterol to become small/dense Particle B. These small/dense lipoprotein particles are small enough to penetrate the arterial wall ( Endothelium). These have the potential to be oxidized, you don`t want that. 8) **Oxidized cholesterol** accelerates the development of atherosclerosis. 9) You want your liver to make LDL cholesterol Particle A large and fluffy. Cholesterol is vital to every cell in your body and is the substrate needed to manufacture most of your hormones. 10) A T2 diabetic (insulin resistant) continues to eat a SAD high carbohydrate diet the excess glucose is send to the liver and the liver must make more of the lipoprotein VLDL. The more fat the liver makes from excess glucose (carbs) the more VLDL cholesterol it needs to make to transport the fat in the bloodstream. 11) If a T2 diabetic would be able to adopt a ketogenic diet and stop this excess flow of glucose to the liver his metabolic health would change dramatically. 12) Dietary fat can be used in place of glucose (Carbs) for most of your energy needs. Dietary fat is much more calorie dense than carbohydrate as fat has 9 calories per gram compared to 4 calories per gram of carbohydrate. 13) Dietary fat has a much different fate in the human body than liver made fat from excess glucose (carbs) 14) If you eat a ketogenic diet and are keto-adapted your cells can now use dietary fat (and your stored body fat) for direct energy. 15) Dietary fat has a totally different lipoprotein transport system that liver made fat, VLDL 16) Dietary fat is sent to your intestines (not the liver) where it is broken down into smaller units by your pancreatic digestive enzymes and re-packaged with the lipoprotein chylomicron. The protein identifier for chylomicron is different that the protein identifier for liver made fat. This protein identifier is APO48. 17) Your hungry cells quickly grab onto this chylomicron (APO48 identifier) and use this dietary fat for direct energy, if keto-adapted. These chylomicrons have a very short half life and these fats will be to few to measure in your fasting blood triglycerides. 18) Do not misunderstand me. I am *not* telling you to shove 2 sticks of butter down the hatch. Just like anything else in the human body you can only handle so much of anything at any given time. Your body has systems in place also for the flow of free fatty acids. 19) What am I trying to tell you with this information? If your a T2 diabetic please stop eating a SAD high carbohydrate diet. Do not fear dietary fat, but do not use dietary fat as a new crutch for your over eating disorder BACKGROUND:The potential role of whole grain in preventing various mortality outcomes has been inconsistently reported in a wealth of prospective observational studies.
OBJECTIVE:We evaluated the relations between whole-grain intake and risks of dying from any cause, cardiovascular disease (CVD), and cancer through a meta-analytic approach. DESIGN:Relevant studies were identified by searching PubMed and EMBASE databases and bibliographies of retrieved full publications. Summary RRs with 95% CIs were calculated with a random-effects model. RESULTS:Thirteen studies on total mortality (104,061 deaths), 12 on CVD mortality (26,352 deaths), and 8 on cancer mortality (34,797 deaths) were included. Three studies reported whole-grain intake, and the remaining studies reported whole-grain product intake. In the dose-response analysis in which the intake of whole-grain products was converted to the amount of whole grain, the summary RRs for an increment in whole-grain intake of 50 g/d were 0.78 (95% CI: 0.67, 0.91) for total mortality, 0.70 (95% CI: 0.61, 0.79) for CVD mortality, and 0.82 (95% CI: 0.69, 0.96) for cancer mortality. A similar reduction was observed for the mortality from ischemic heart disease (RR: 0.68; 95% CI: 0.55, 0.84) but not from stroke (RR: 0.93; 95% CI: 0.54, 1.62). There was evidence of nonlinear associations of whole-grain intake with total (P-nonlinearity < 0.001) and CVD mortality (P-nonlinearity <0.001), but not with cancer mortality (P-nonlinearity = 0.12), with the curves for the associations appearing slightly steeper at lower ranges (<35 g/d) of the intake than at higher ranges. CONCLUSIONS:Our findings suggest significant inverse relationships between whole-grain intake and mortality due to any cause, CVD, or cancer. The findings support the recommendation of increasing whole-grain intake to improve public health. Source: http://www.ncbi.nlm.nih.gov/pubmed/27225432  On May 20, 2016 the FDA finalized the new Nutrition Facts label for packaged foods. Among some other minor changes, the FDA is requiring food manufacturers to identify all “added sugars” in food products. Previously, these added sugars were lumped in with the “Total Carbohydrates” section of the label, and only naturally occurring sugars were identified. “Total Sugars,” in the past, have included added sugars, but this new label will expose those added sugars on an additional section of the label. Manufacturers will need to implement this new label by July 26, 2018. However, manufacturers with less than $10 million in annual food sales will have an additional year to comply. Here’s a glimpse at the new label changes: The FDA recommends that Americans consume less than 12.5 teaspoons of added sugars per day. The average American consumes 60% more sugar than that allowance. Many health organizations believe that the daily limit of added sugar intake should be as little as 6 teaspoons per day. Though these new regulations are still based on a macro-nutrient ratio that is completely out of whack, they are at the very least, a step in the right direction. I would imagine it’s difficult to squabble over the US daily allowance for added sugars with a government organization that still thinks Kellogg’s frosted flakes are healthier than an avocado. There are many reasons that processed food companies started utilizing “added sugars” in the production of their products. Due to an alarming rise in incidents of fatal heart attacks and heart disease in the late 70s, the US government implemented the dietary guidelines for America that mandated a reduction in dietary fats. This change was based on research that had not been proven, and was concocted by unqualified legislators instead of Nutritional Scientists. The food companies then had to reformulate their recipes to accommodate these new guidelines. The reduction and/or removal of dietary fat required that they be replaced by one of, or a combination of the two remaining macronutrients. Since many sources of fat were also rich with protein, the addition of carbohydrates was the only logical choice to fill that void. Sugar, being the Queen Mother of all carbohydrates, also happened to be delicious. The food companies discovered that the addition of sugars would not only improve taste, texture and palatability, but also improve shelf life. Scientific studies have indicated that “added sugars” also enhances addict-ability, which would obviously improve profitability. All of this to the unfortunate detriment of the public health. Sugars are undisputedly the main contributor to the obesity/diabetes epidemic that has plagued our country for the last three decades. This video illustrates the situation in a brief, yet entertaining way: Processed food companies have become notorious for taking liberties with the truth in an effort to hide the existence of these added sugars from the consumer. Some of the language used on food labels would be more appropriate in the urban dictionary than on a list of ingredients. Their attempts at hiding “added sugars” on food labels have been nothing short of comical. As far as I can tell, there are nearly 300 different words being used to describe sugar on food labels in the US (a liberal estimation). Listed below are some of the most common: Agave, Agave nectar, Anhydrous, Caramel, Carbitol, Corn sweetener, Crystalline fructose, Barley malt, Dextran, Dextrose, Diastatic malt, Diglycerides, Disaccharides, Diastase, Erythritol, Ethyl maltol, Florida crystals, Fructooligosaccharides, Fructose, Fructose crystals, Galactose, Glucitol, Glucoamine, Glucose, Glucose solids, Hexitol, Honey, Inversol, Isomalt, Lactose, Malt, Maltodextrin, Maltose, Mannitol, Muscovado, Nectar, Panocha, Pentose, Sorbitol, Sorghum, Sucanat, Sucanet, Sucrose, Treacle, Xylitol, Xylose, Zylose. Cane juice, Cane juice solids, Dehydrated cane juice, Evaporated cane juice, Fruit juice, Fruit juice concentrate, Fruit juice crystals, Fruit juice solids, {enter fruit name here} juice. Barbados sugar, Beet sugar, Brown sugar, Cane sugar, Coconut sugar, Confectioner’s sugar, Castor sugar, Date sugar, Demerara sugar, Evaporated sugar cane, Free Flowing Brown Sugars, Golden sugar, Granulated Sugar, Grape sugar, Glazing sugar, Icing sugar, Invert sugar, Malt sugar, Maple sugar, Organic raw sugar, Powdered Sugar, Raw sugar, Table sugar, Turbinado sugar, White sugar, Yellow sugar Buttered syrup, Corn syrup, Corn syrup solids, Carob syrup, Evaporated cane syrup, Golden syrup, Glucose syrup, High Frustose Corn Syrup, King’s syrup, Malt syrup, Maple syrup, Molasses, Raisin syrup, Refiner’s syrup, Rice syrup, Sorghum syrup. Will the FDA’s new Nutrition label lead to a whole new wave of trickery by the food companies? …oh, you betcha! Now that the FDA has issued a moratorium on “added sugars” with their required inclusion on product labels, the food companies are going to have to get even more clever when attempting to hide their existence from the general public. Since the FDA’s announcement in 2014, many (most) food companies have been lobbying feverishly to squash these new regulations, but to no avail. Now they have no other recourse than to squabble over the minutia. One sugar lobby has already confronted the FDA with the claim that the teaspoon is a misleading unit of measurement. While another claims that grams are confusing. Let there be no doubt, the food companies will be doing everything within their power to blur the lines as to what “added sugars” actually are. What’s next? Sugar accounts for a small fraction of U.S. farm output, but the industry contributes more to congressional campaign coffers than any other commodity producer. According to the Center for Responsive Politics, between 2007 and 2015 growers donated more than $22 million. They have money, and they are not afraid to spend it. The sugar lobby’s power and influence should not be underestimated. They will most certainly be wielding cash to discover/create loopholes that we haven’t even thought of yet. “There is likely to be litigation over what is and isn’t added sugar,” said Stephen Gardner, an attorney at the Dallas-based Stanley Law Group and former director of litigation at CSPI. A case will likely be made that sugar additives that are naturally occurring in nature, or that contain a slight modicum of minerals should not be counted amongst added sugars. Professor Jeremy Kees, a nutrition label expert from Villanova University School of Business, who has consulted for both the FDA and the food industry, said that he believes that the label change will have a relatively small impact on consumers, “I think front of pack labeling has more potential to have a bigger impact on consumers.” Blurring the lines with buzz words All natural, All natural ingredients, Natural, Organic, Pure, Raw, Unrefined, Wholesome, DOES NOT mean “healthy“. You’re going to be seeing this terminology used at nauseum. These words will likely be used liberally on front label packaging containing “natural” sweeteners. The sugar lobby will argue that sweeteners that come from fruit and other natural sources should not be counted as added sugars. The problem is, the sugar that comes from fruit and most other natural sources is just NOT healthier, NOT different in any substantive way from the sugar that comes from sugarcane. This misunderstanding is exactly how food producers will exploit this rule. They will add apple juice or agave to everything that kids eat, and then their product will technically have no “added sugars,” even when they actually have loads of added sugars. Food companies would like nothing more than to trick you into believing that their product is somehow wholesome, or “good for you” just because it’s sweetened naturally. The term organic is only regulated currently by the USDA, for the production of meats, poultry and eggs only. The FDA has no regulation for the use of the term organic and neither organization has implemented hard fast rules for the use of the word natural. ” … but it’s all natural!” You say … Oh yeah, well so is cyanide. “How bout a nice little poison ivy salad with some cow dung mushrooms, black mold croutons and a crude oil dressing? Perhaps you could wash it down with a lovely poison oak tea? …“ …why not, it’s natural?!! Did you know that 97% of the vegetation that grows on the planet is not fit for human consumption, and it’s all natural. Here’s a breakdown of some of the natural sweeteners that the health food community often claim are healthy: Agave (nectar or syrup) – A very popular sweetener in the natural health community. This sweetener is often considered a healthy alternative to sugar because it’s low on the glycemic index. The harmful effects of sugar have little to do with the glycemic scale, and everything to do with the fact that Agave is very high in fructose content. Repetitive fructose consumption can lead to insulin resistance which will chronically elevate blood sugar and insulin levels. Sugar is nearly 50% fructose, while Agave contains 70-90% fructose, far worse than sugar gram for gram. Raw Organic Cane Sugar – Many so called “health products” are sweetened with raw, organic sugar. Organically grown sugar has the same chemical composition as “regular” sugar. The fact that it “raw” or how it’s processed means nothing, our bodies metabolizes it in exactly the same way. Evaporated Cane Juice – This one always makes me laugh. Do food companies really think that describing the way the Cane Sugar is processed is going to make it sound healthier? This one is just deception plain and simple. Evaporated cane juice IS sugar. Brown Sugar – Molasses forms as a by-product of the sugar refining process and is often added back in small amounts giving the sugar a brown color. Molasses is about 50% sugar and contains a small amount of minerals. Brown sugar is regular sugar diluted with a slightly less unhealthy, less concentrated sugar. The tiny amount of minerals hardly make up for it’s contribution towards insulin resistance. Coconut Sugar – Derived from the circulating fluid of the coconut plant.The processing method is very natural… it simply involves extracting the fluid, then allowing the water to evaporate. Coconut sugar contains a small amount of fiber and a few nutrients, also has a lower glycemic index than regular sugar. However, the glycemic index is just shy of irrelevant when it comes to the harmful effects of sugar. What really matters is whether this product is high in fructose or not. Coconut sugar is actually very high in fructose. It contains a small amount of free fructose, but 75-80% of it is sucrose, which is half fructose. That’s about 35-45% total fructose. Due to its slightly smaller amount of fructose than sugar, and the tiny amounts of fiber and nutrients, you could say that coconut sugar is less unhealthy than regular sugar, gram for gram. However… being “less unhealthy” than sugar does NOT make it healthy. Honey – Contains some nutrients which includes antioxidants and trace amounts of vitamins and minerals. However, it is 80% sugar, by weight. Several studies have compared honey to plain sugar and noted that honey has slightly less harmful effects on metabolism. This is yet another example of a sweetener that is slightly “less unhealthy” than sugar. While a better choice than high fructose corn syrup, it is not recommended if your goal is weight loss. The Bottom Line: Your body metabolizes the fructose in all of these natural sugars the SAME way as it does with regular sugar. Your liver doesn’t know the difference! I know what you might be thinking …is this the part in the article where he reminds us that we can satisfy our sweet-tooth with fiber rich fruits and berries? Is this just a full on assault on all things sweet? Must we live our days tasting only saltiness, sourness and bitterness if we want to eat healthy? Have we been presented with a problem that has no solution? Does the food industry even have healthy options for added sugar? What’s with all the questions? I think both Doctors and Dietitians would agree that a healthy diet would exclude eating processed foods that are subject to added sugars in the first place. The foods products that are designed and formulated to target children are most egregious offenders in this battle against added sugars. Sugar IS an addictive substance and that’s not just an opinion, that’s a fact. 1 out of every 3 children between the ages of 2 and 19 are overweight. These children have a 70% chance of becoming obese adults. THE FACT OF THE MATTER IS: The food companies DO have healthy (or at least “not unhealthy”) options in regards to the added sugars they use in their products! Here is a short list of some of the most common “not unhealthy” sweeteners: Stevia – A very popular low-calorie sweetener that currently holds a 13% share of the artificial sweetener market in spite of the fact that it is not artificial. It is extracted from the leaves of a plant called Stevia rebaudiana. This plant has been grown for sweetness and medicinal purposes for centuries in South America. There are several sources of sweetness found in Stevia leaves, the main ones are Stevioside and Rebaudioside A. Both are many hundred times sweeter than sugar, gram for gram, with virtually no calories. There have been several studies conducted with humans revealing Stevia to have health benefits. When blood pressure is high, Stevia can lower it by 6-14%. However, it has no effect on blood pressure that is normal, or only mildly elevated. Stevia has also been shown to lower blood sugar levels in diabetics. There have also been studies in rats showing that Stevia can improve insulin sensitivity, reduce oxidized LDL cholesterol, and reduce plaque build up in the arteries. Stevia also has the greatest consumer availability than most of the other safe sugar replacements. Erythritol – is low-calorie sweetener. It’s a sugar alcohol that is found naturally in certain fruits It contains 0.24 calories per gram, that’s about 6% of the calories that sugar has, with 70% of the sweetness. Erythritol doesn’t spike blood sugar or insulin levels and has no effect on biomarkers like cholesterol or triglycerides. It is absorbed into the body from the intestine, but is excreted from the kidneys unchanged. Studies show that erythritol is very safe. However, same as with other sugar alcohols, it can cause digestive issues if you consume too much at a time. Erythritol tastes very much like sugar, although it can have a mild aftertaste. Xylitol – is a sugar alcohol with a sweetness similar to sugar. It contains 2.4 calories per gram, or about 60% of the caloric value of sugar. Xylitol has some benefits for dental health, reducing the risk of cavities and dental decay. It has also been attributed to improved bone density, helping to prevent osteoporosis. Xylitol doesn’t raise blood sugar or insulin levels. However, as with other sugar alcohols, it can cause digestive side effects if consumed in high doses. Xylitol is toxic to dogs, but completely safe for humans. Yacon Syrup – is harvested from the Yacon plant, which is native to the Andes in South America. This sweetener has recently become popular as a weight loss supplement because one study found that it caused significant weight loss in overweight women. It is high in fructooligosaccharides content, which functions as a soluble fiber that feeds the good bacteria in your intestines. Yacon syrup can help reverse constipation. Monk fruit (luo han guo) – is a fruit native to China and northern Thailand. It’s 300 times sweeter than sugar, and has been used in traditional Chinese medicine to treat obesity and diabetes. Luo han guo is a cousin of the cucumber, and contains mongrosides. Studies are underway to discover whether there is truth to the claim that these monogrosides inhibit tumor growth. Luo han quo has antioxidant properties, and may help manage diabetes. Because these antioxidants have inhibitory effects on blood sugar levels, they may also defend against heart disease. Teas made from luo han guo have been known to relieve throat inflammation or cough, cool heat stroke, help with elimination in the elderly, and aide in the relief of digestive distress. The Bottom of the Bottom Line: The Food Industry DOES in fact have healthy/not unhealthy options in regards to the use of added sweeteners to improve the palatability of their processed foods. The real question is – Will they utilize their considerable resources ($) to litigate in an effort to maintain the status quo? Will they direct their money towards developing and improving upon the use, production and implementation of healthier options? Though the most likely scenario is a combination of both (skewed heavily on the side of litigation) my hope is that the FDA will stand strong and not allow politics to influence the ingredients included in products targeting our country’s children. Bladder Pain Syndrome or interstitial cystitis is a disabling chronically painful condition mostly in women that affects all parts of one’s life. The cause is unknown, the treatments few and effectiveness poor.
We have good evidence that CBD reduces all inflammatory cytokines seen in BPS, including IL1, 6 and 8 as well as IL-17. On top of this, CBD blocks the CB1 receptor activation which has been shown to be involved precisely in this condition. Thus, there is every reason t...o believe CBD could be highly effective improving the lives of women and men with this terrible affliction. The exact amount of CBD needed has not been studied or reported but based on clinical responses for other conditions a suggested amount might be 30 mg per day. Ref: J Neuroinflammation. 2016 Jun 3;13(1):136. J Urol. 2014 Nov;192(5):1564-8. Am J Pathol. 2010 Jan;176(1):288-303. Int J Urol. 2016 May 24. |



 RSS Feed
RSS Feed
